Integrated Care Pathways for HIV patients


We work in close collaboration with the NHS Lothian and NHS Greater Glasgow and Clyde boards to improve HIV care by mapping the processes involved in the form of an Integrated Care Pathways (ICPs). We employ a rigorous methodology involving contextual interviews, questionnaires, and shadowing to capture the and record necessary knowledge. Using the logic-based tool WorkflowFM for this purpose offers the following advantages:
- An intuitive, diagrammatic visualisation of the care pathways which helps clinicians better understand their own practices, analyse and rethink them.
- The use of a structured data model facilitates the recording and versioning of these models so that they can be more easily maintained and evolved as policies and practices change. They can also be shared to amongst the different stakeholders to enable collaborative development, as well as across sites for a fruitful comparison.
- Formal verification techniques mechanically check the correctness and consistency of our models. This can help eliminate errors, increase the trustworthiness of the model, and improve patient safety.
- Executable code (including for example workflow automation and generated checklists) can be extracted from these models to form an optimised social machine for healthcare provision.
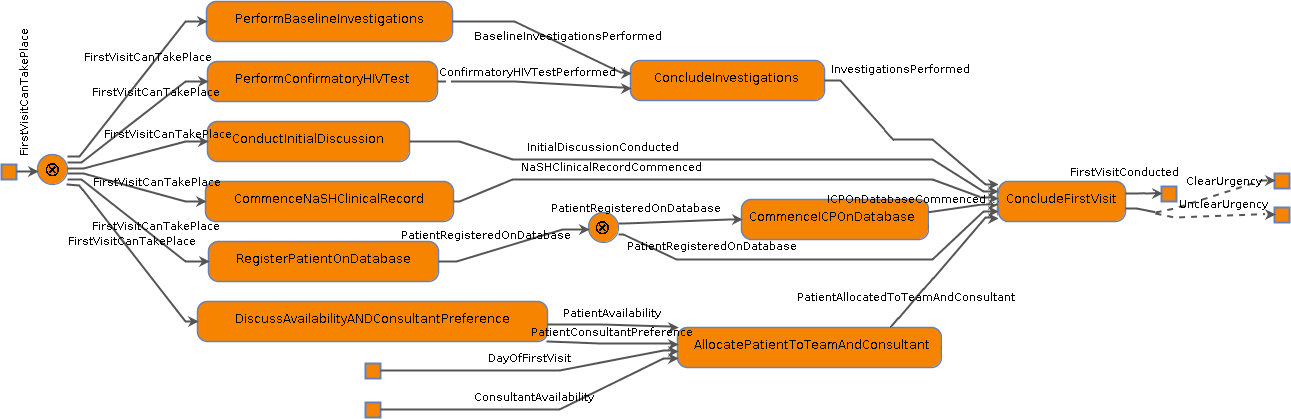
Figure 1: Workflow for the first visit after diagnosis for new HIV patients.
Our work aims to extend and enhance this mapping by formalising care workflows using our logic-based tool WorkflowFM. We focus particularly on actors, resources and workflows involved in the first 3 months of HIV care for the Chalmers Sexual Health Centre. The resulting models and analysis can help address some of the difficulties faced by units providing HIV outpatient care. In short, we believe process-based workflow models can be an effective methodology to document and share care pathways provided they are developed in close collaboration with clinical stakeholders.
This research was partially supported by EPSRC grant EP/N014758/1.
